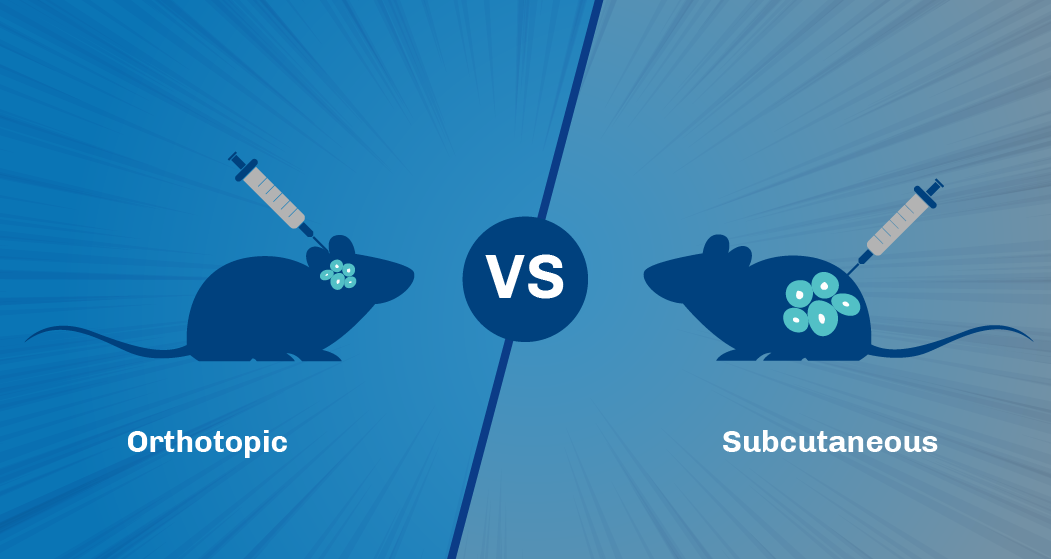
The scientific community has long appreciated the importance of in vivo tumor models for understanding cancer biology and testing therapeutic strategies. Two popular methods for tumor implantation in these models are orthotopic and subcutaneous implantation. Both have their advantages, and the choice often depends on the specific goals of a study. In this post, we'll delve deep into the benefits of each method to guide researchers in their decision-making process.
Orthotopic Implantation
Advantages:
- Tumor Microenvironment: Implanting the tumor in its tissue of origin (e.g., liver tumors in the liver or brain tumors in the brain) better represents the natural microenvironment, offering insights into tumor growth, invasion, and metastasis in a more clinically relevant setting.
- Metastatic Potential: Orthotopically implanted tumors show a higher tendency for metastasis, vital for studies focusing on metastatic processes or testing drugs targeting metastatic cells.
- Treatment Response: Since the tumors are in their natural environment, they might respond more similarly to therapies as they would in humans, providing a more accurate representation of potential clinical outcomes.
- Advanced Imagining Compatibility: Orthotopic models, especially with the right equipment, allow for detailed imaging studies. The tumor’ location in native tissues can enable more precise imaging and visualization techniques, providing deeper insights to tumor growth, angiogenesis, and drug response.
Limitations:
- Technical Complexity: Orthotopic implantations can be technically demanding, requiring specialized skills, especially when implanting tumors in challenging locations like the brain or pancreas.
- Variability in Tumor Take: Depending on the tissue type and cell line, there can be variability in the “take rate” or successful engraftment of the tumor. This inconsistency might necessitate more animals or samples to achieve statistical significance in some studies.
- Higher Costs: Due to the need for specialized equipment and expertise, orthotopic implantation might be more expensive than subcutaneous implantation.
When to Choose Orthotopic Implantation:
Orthotopic implantation stands out when the focus is on understanding the tumor’s interaction within the context of the native environment, including the relationship with stromal cells, immune cells, and the extracellular matrix. Researchers keen on unraveling metastatic mechanisms or evaluating therapeutic agents targeting metastasis will find this method particularly beneficial. Moreover, orthotopic models are invaluable when the objective is to assess how a tumor responds to treatments in indication specific locations, especially when findings might transition to clinical trials. Additionally, studies equipped to use advanced imaging techniques to track tumor growth—given the inherent challenges of monitoring tumors in orthotopic sites—will benefit greatly from this approach.
Subcutaneous Implantation
Advantages:
- Ease of Implementation: This method involves the introduction of tumor cells into the subcutaneous space, typically in the flank of the animal. Due to its accessibility, subcutaneous implantation is technically easier and faster than orthotopic procedures.
- Tumor Measurement: Tumors implanted subcutaneously are easily palpable, allowing for straightforward monitoring of tumor growth by simple caliper measurements.
- High Success Rate: The subcutaneous model often yields a high take rate, requiring fewer animals and making it more predictable for study outcomes.
- Cost-Efficient: Less technical expertise is required, translating to quicker procedures and reduced costs.
Limitations:
- Anatomical Differences: The subcutaneous environment might not accurately reflect the native tissue from which the tumor originated. This can affect tumor behavior and responsiveness to treatments.
- Absence of Metastasis: Subcutaneous models are less likely to metastasize compared to orthotopic models, which limits its use in studies where metastasis is the primary aim.
- Lack of Vascularization: Subcutaneous tumors might not develop the extensive vascular network seen in orthotopically implanted or naturally occurring tumors. This could impact drug delivery and tumor microenvironment interactions in certain studies.
- Inconsistent Drug Responses: Some therapeutics especially those targeting specific organ environments or systems, might not elicit the same response in subcutaneous models as they would in orthotopic models or human conditions.
When to Choose Subcutaneous Implantation:
Subcutaneous implantation is ideal for preliminary studies, such as gauging the tumorigenic potential of a cell line or assessing a drug's antitumor efficacy at an early stage. Its ease of monitoring makes it especially suitable for projects that prioritize straightforward, non-invasive tracking of tumor progression. Additionally, if a study operates under budget constraints and requires a more cost-effective approach without compromising basic tumor growth aspects, subcutaneous models are a go-to. This method is also adequate for short-term studies that don’t delve into in-depth interactions or metastatic behaviors.
Conclusion
While both orthotopic and subcutaneous implantations offer unique advantages, the choice between them should be based on the specific objectives of the study. For research focused on general tumor growth or initial drug screening, subcutaneous models might be preferable. Conversely, for studies requiring a more clinically relevant model, especially those focused on metastasis or tumor environment interactions, orthotopic implantation is the preferred model.
Understanding the strengths and limitations of each method ensures that researchers can select the most appropriate model, optimizing the translatability and relevance of their findings.